Program Philosophy
The nursing education philosophy recognizes that students have individual learning needs, learning styles, readiness, support systems, and cultural and ethnic backgrounds. Learning is a continuous, life-long process that occurs in the affective, cognitive and psychomotor domain, proceeding from simple to complex and enhanced by an environment that motivates the student to apply the theory to practice using critical thinking, evidence based practice, informatics, clinical simulation experience, patient-centered care, and the nursing process.
The faculty use diverse teaching strategies to meet the varied learning styles and learning needs of our diverse students. Faculty are committed to assisting all students to achieve their professional goals by providing a supportive environment for learning and personal growth in an accessible learning environment. Student support programs are utilized to assist students in achieving academic success from entry to graduation.
Education of the nurse at the Associate Degree level prepares the individual as an entry level nurse in the profession of nursing. The nurse is educated to provide safe, competent, caring interventions, and patient care management through sound clinical decision making, communication, and leadership. Integrity, respect for the individual, ethical behavior, accountability, lifelong learning are attributes of the art and science of nursing care.
The faculty believe that nursing as a profession is an art and science as well as practice discipline that responds to society’s health needs in a caring manner in a variety of environments.
As a scientific discipline, nursing draws on a discrete body of knowledge that incorporates an understanding of the relationships among nurses, patients, and environments within the context of health, nursing concepts and theories, and concepts and theories derived from the basic sciences, humanities, and other disciplines. The science of nursing is applied in practice through a critical thinking framework known as the nursing process that is composed of assessment, diagnosis, planning, implementation, and evaluation. The steps of the nursing process serve as a foundation for clinical decision-making and evidence-based practice. Nurses use critical thinking to integrate objective data with knowledge gained from an assessment of the subjective experiences of patients and groups, and to apply the best available evidence and research data to the processes of diagnosis and treatment. Nurses use clinical reasoning to respond to the needs of the populations they serve. Nurses develop and communicate strategies to support optimal outcomes that are most appropriate to the patient or situation while being mindful of resources utilization. Nurses continually evaluate the quality and effectiveness of nursing practice and seek to optimize outcomes (American Nurses Association [ANA], 2004.
The art of nursing is based on a framework of caring and respect for human dignity. The art and science of nursing are inextricably linked, as a compassionate approach to patient care carries a mandate to provide care competently and within a systems-based practice. Competent care is provided and accomplished through delegated, independent and interdependent practice (Koloroutis, 2004, pp. 123-25), and through communication as well as collaborative practice (Tomey, 2009, p. 397) involving other colleagues and/or the individuals seeking support or assistance with their healthcare needs (ANA, 2004, p. 12).
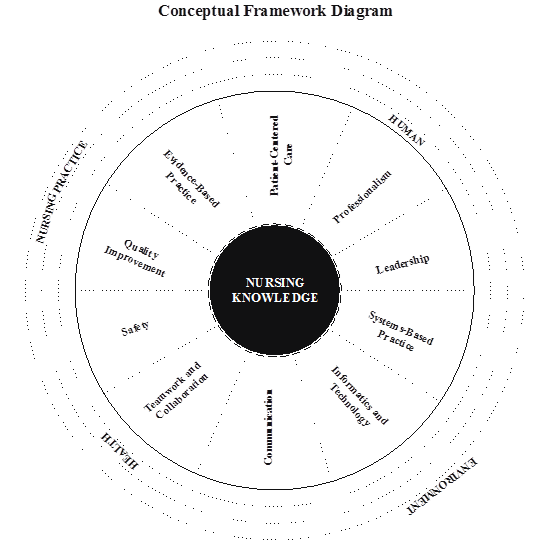
The distinctive focus of the discipline of nursing is on nursing actions and processes, which are directed toward human beings and take into account the environment in which individuals reside and in which nursing practice occurs (Fawcett & Garity, 2009). This distinctive focus is reflected in the metaparadigm of nursing, which identifies human beings (patients), the environment, health, and nursing as the subjective matter of interest to nurses (ANA, 2004). In the context of nursing knowledge, these constructs are defined as follows:
Human beings/patients – the recipient of nursing care or services. This term was selected for consistency and recognition and support of the historically established tradition of the nurse-patient relationship and recipients of nursing care. Patients may be individuals, families, groups, communities, or populations. Further, patients along the health-illness continuum may function in independent, interdependent, or dependent roles, and may seek or receive nursing interventions related to disease prevention, health promotion, or health maintenance, as well as illness and end-of-life care. Depending on the context or setting, patients may at times more appropriately be termed clients, consumers, or customers of nursing services (AACN, 1998, p. 2).
Environment – an open and evolving system consisting of internal and external factors, such as physical, psychological, social, cultural and spiritual influences that affect the life, health, and survival of a person or community. The person interacts and communicates with the environment. The nurse achieves patient outcomes by providing a safe and effective health care environment in order to protect patients, families, groups, and other health care personnel within the context of community.
Health – an experience that is often expressed in terms of wellness and illness, and may occur in the presence or absence of disease or injury (ANA, 2004, p. 48).
Nursing – is the protection, promotion, and optimization of health and abilities, prevention of illness and injury, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, groups, communities, and populations (Retrieved ANA, 8-30-2015).
Core Concepts
The core concepts emanate from the foundation of nursing knowledge. The concepts consist of the following:
- Patient-Centered Care
- Professionalism
- Informatics and Technology
- Evidence-Based Practice
- Leadership
- Systems-Based practice
- Safety
- Communication
- Teamwork and Collaboration
- Quality Improvement
See model.
Figure 1 : The model is a graphic representation of the core concepts and their relationship to nursing knowledge. In the model, nursing knowledge has been placed at the core to represent how nursing knowledge in its totality reflects the overarching art and science of the nursing profession and discipline. The ten essential concepts, which guide nursing curricula and practice, emanate from this central core and include patient-centered care, professionalism, leadership, systems-based practice, informatics and technology, communication, teamwork and collaboration, safety, quality improvement, and evidence-based practice. The order of the concept does not indicate any hierarchy, as all the concepts are of equal importance. The concepts are connected by broken lines because distinction between individual concepts may be blurred; the concepts overlap and are not mutually exclusive. The concepts are similarly connected to the core by a broken line to indicate the reciprocal and continuous relationship between each of the concepts and nursing knowledge.
Adapted from Massachusetts Nurse of the Future 2016
Program Student Learning Outcomes
Graduates of the Ventura College ADN Program will demonstrate the following:
- Provide safe, quality, culturally appropriate, patient-centered care to patients, families, and groups supported by evidence-based clinical decisions and patient preferences in a variety of settings.
- Communicate effectively with patients and members of the inter-professional health care team to provide and coordinate safe, quality, patient-centered care.
- Demonstrate leadership and system management knowledge and skills in the delivery of quality health care to patients while contributing to the effectiveness and efficiency of the work unit.
- Integrate established regulatory (California Nurse Practice Act), legal and ethical principles into standard-based professional nursing practice.
Evidence that graduates have learned the knowledge, skills and ethical basis for nursing practice is not only reflected in student accomplishment of level competencies, but also:
- Performance on the NCLEX licensure examination
- Program completion
- Program satisfaction
- Job placement